Believe it or not, the Electronic Health Record (EHR) is not a new concept. Though it was previously referred to as an Electronic Medical Record (EMR) or Computerized Patient Record (CPR), it was first validated all the way back in 1991. Experts knew then and they know now – it’s one of the pieces needed to completely transform the medical care system if we want to boost quality and improve safety.

Back to the basics: What is an EHR?
Put simply, an EHR is a digital version of a medical record. It’s maintained by the provider over time and includes all the data relevant to each patient, including notes from their doctor, diagnoses, vital signs, immunizations, radiology reports, and all other pertinent data. Use of an EHR automates access to this vital information and allows numerous physicians to get instant access to the details they need.
There are many benefits to implementing an EHR, including:
- Lowering medical error by boosting accuracy and clarity in medical records
- Making health care information readily accessible
- Reducing test duplication
- Lowering delays in treatment
- Better informing patients
The main drawback of implementing an EHR is the cost involved in moving from paper records to digital files. Some health care offices simply don’t want to make the leap to an upgraded system. Many doctors who are interested in implementing this use a virtual office or a bpo provider to help accomplish this.
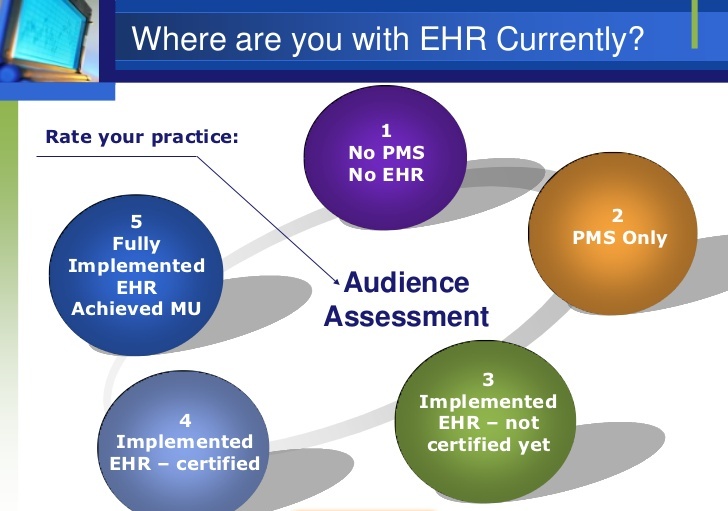
Should your practice implement EHRs?
The first step in implementing is deciding if you should implement an EHR in the first place. Work with the decision makers at your offices to ask these important questions:
- Are we accomplishing what we set out to accomplish when we went to medical school?
- Are our patients getting the best possible care from us?
- What would we do differently if we had more time?
- What would it be like if we could leave the office but stay connected to the practice?
- Are our administrative processes efficient, organized, and well documented?
- Is data collected and reported in consistent ways?
- Are staff members up to date on the latest technology?
- Do we have specialty specific requirements?
Consider your long-term and short-term goals, financial readiness, and willingness to take on new technology.
Set specific goals for implementation
Your practice needs goals to help guide everyone through the various decision-making steps of implementing your EHR. You may need to reassess these goals as you walk through the process. To begin with, think about which goals are most important to you. Are you concentrating on revenue, specific clinical care goals, or improving your work environment? The SMART goal process offers a simple guide map to creating and meeting goals. According to it, every goal should be:
- Specific. Make sure every goal you identify could make a difference for either your patients or your practice.
- Measureable. A good goal is one that can be quantified.
- Attainable. You do want to stretch to reach your goals, but at the end of the day, they must be attainable.
- Relevant. Every goal you set must be worth the effort.
- Time bound. Create goals with specific timelines.
Following these criteria will help your practice begin the process of implementing an EHR and achieving your goals.
Outcomes of your assessment process
After you’ve completed a comprehensive assessment you will have gathered more information that can be used to move forward with the process. Some outcomes of this assessment should be:
- Designated team in charge of implementation. You need leadership who can step up and handle the EHR implementation process. For larger offices this may include clinical and practice management staff, while in smaller practices it may include the entire team. Regardless of the number of people on the team, remember that having strong, clear, positive advocators for needed change can be one of the most useful tools in your transition.
- Unified vision. Every member of your team should understand how they’ll be affected by the change, the roadmap for implementation, and the results of the change.
- Measureable, realistic, quantifiable goals. The clearer your goals are, the clearer your roadmap to achieve them will be.
Implementing an EHR is a cost-effective option to provide better care to every patient. The above steps will help your practice get on track with the implementation process.